Polyarteritis Nodosa (PAN) and Perinuclear Anti-Neutrophil Cytoplasmic Antibody (p-ANCA) relate to each other in the context of vasculitis, specifically in how PAN is diagnosed and differentiated from other similar conditions. Here’s an explanation:
Polyarteritis Nodosa (PAN):
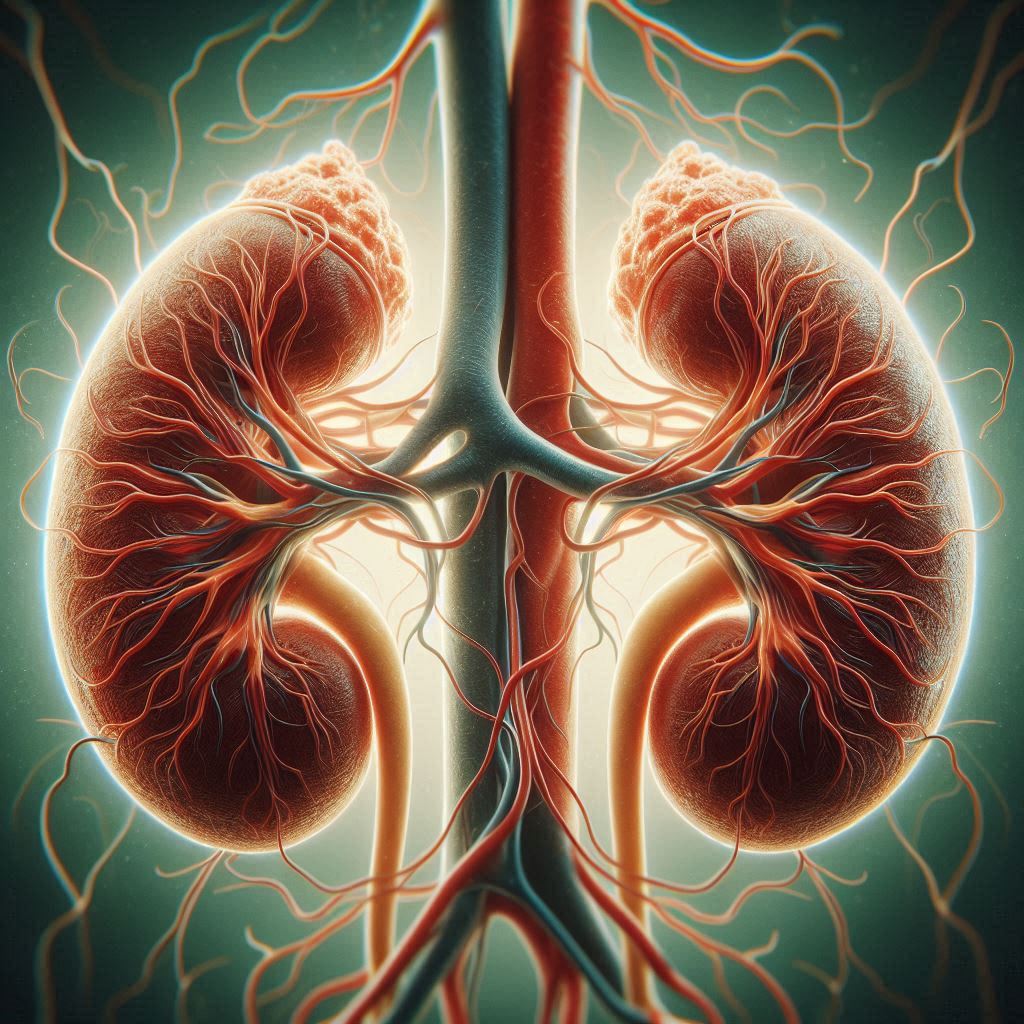
- Definition: PAN is a systemic necrotizing vasculitis that predominantly affects medium-sized arteries, although it can involve small vessels too. It’s characterized by inflammation of the arterial walls, leading to aneurysms, thrombosis, and organ ischemia.
- Symptoms: Can include fever, weight loss, muscle and joint aches, skin lesions, peripheral neuropathy (often mononeuritis multiplex), hypertension due to renal artery involvement, and gastrointestinal symptoms like abdominal pain or bleeding.
- Diagnosis: Typically, PAN does not associate with ANCA, particularly p-ANCA, in its classic form, distinguishing it from other vasculitides like microscopic polyangiitis (MPA). Diagnosis is often based on clinical presentation, biopsy showing vasculitis, and sometimes angiography revealing aneurysms or vessel narrowing.
Perinuclear Anti-Neutrophil Cytoplasmic Antibody (p-ANCA):
- Definition: p-ANCA refers to a type of ANCA where immunofluorescence shows a perinuclear staining pattern. It’s often associated with antibodies against myeloperoxidase (MPO), but not exclusively.
- Association with PAN: Historically, PAN was not considered to be associated with ANCA, especially p-ANCA. However, there are exceptions:
- Microscopic Polyangiitis (MPA): This condition, which can resemble PAN, typically features p-ANCA positivity, especially with MPO specificity. MPA affects smaller vessels and can involve the lungs and kidneys, which is less common in classic PAN.
- Atypical Cases: Some cases of PAN might show low-level p-ANCA positivity or be associated with other forms of vasculitis where p-ANCA can be present, leading to diagnostic confusion.
- Clinical Implications:
- The absence of p-ANCA supports the classic diagnosis of PAN, particularly when clinical and histopathological findings align.
- The presence of p-ANCA might prompt consideration of MPA or suggest a need for further differentiation from other ANCA-associated vasculitides, although it does not rule out PAN entirely.
Key Points:
- Classic PAN: Generally not associated with p-ANCA; diagnosis is more about clinical and angiographic findings.
- Overlap and Variants: There can be overlap where p-ANCA positive vasculitis mimics PAN, or in some cases, PAN might be associated with low-level p-ANCA, although this is less common and not typical.
- Differential Diagnosis: When p-ANCA is positive, one must consider other conditions like MPA, especially if there’s kidney or lung involvement, which is more characteristic of MPA than PAN.
In summary, while classic PAN is not typically associated with p-ANCA, there can be scenarios where p-ANCA positivity complicates the diagnosis, necessitating a comprehensive evaluation including clinical symptoms, lab tests, and possibly biopsy or angiography for accurate diagnosis.

Leave a Reply